The Asian & Pacific Islander Wellness Center (A&PI Wellness Center) partnered with TechChange to develop a two-part training course designed for clinical and non-clinical providers to provide HIV education in California. For the first time ever, these trainings combined both the self-paced and facilitated course structures. Participants will be asked to proceed at their own pace through the Articulate Storyline-based APIWC 101 course, before taking part in the four-week facilitated course that features chats with guest experts.
HIV Today – The Context
We have come a long way when it comes to HIV treatment. Thirty years of research and campaigns have transformed HIV from being a death sentence into a chronic condition that permits those who properly manage it to live relatively normal lives. The problem is, only one in four HIV-positive Americans currently follow all recommendations for managing HIV.
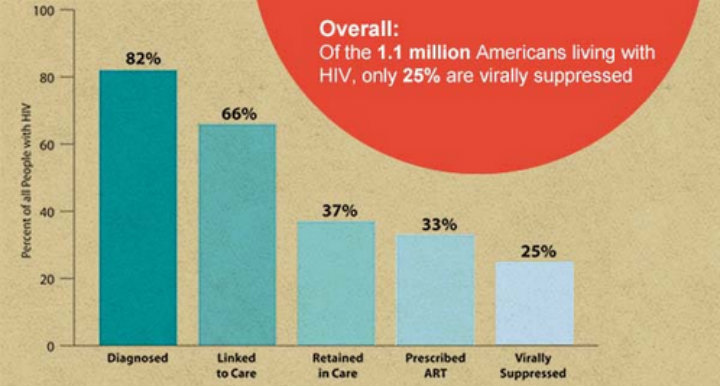
According to the Center for Disease Control (CDC), only 25% of HIV-positive Americans reach viral suppression, the current end-goal of HIV treatment. This means that the other 75%, or roughly 825,000 of the 1.1 million Americans estimated to be HIV-positive, are not receiving the support they need to successfully navigate through the obstacles to seek care. As a result, these individuals are not getting the treatments they need to manage and maintain their personal health and consequently, have a greater risk of transmitting the virus to others.
Many agencies have encouraged use of the HIV Care Continuum, also called the HIV Treatment Cascade, as a tool to visualize the proportion of HIV-positive individuals engaged at each stage of care.
Source: AIDS.gov
This cascade shows an estimated percentage of how many people fall out of care at each step along the way to viral suppression. Nearly one in five HIV-positive Americans do not know their positive status, keeping them from engaging in the cascade at all. Of those that are initially linked to care, nearly half fall out of treatment before being prescribed antiretroviral therapy (ART).
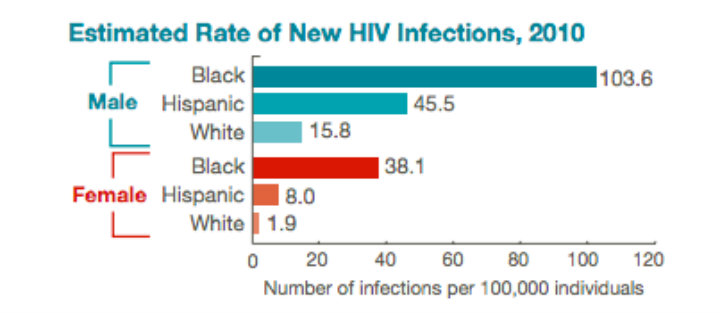
Even more important than this cascade is the breakdown of HIV prevalence by race and sexual preference. African Americans, for example, bear the biggest burden. According to a 2013 CDC report, African Americans makes up 14% of the US population, accounting for 44% of Americans living with HIV. The burden is similarly unequal for other minorities and men who have sex with men (MSM).
source: CDC
These statistics highlight the need for responses tailored to the communities most affected by HIV; these groups are more likely to face poverty and racism, as well as distrust with the medical system. When societal challenges are combined with the challenges of navigating HIV, people tend to drop out of care. Diverse communities require varied responses that are culturally aware and take into account the needs of disenfranchised groups.
The Challenge of Scaling HIV Prevention
Response to HIV requires service providers to play clinical and non-clinical roles. Many counselors, social workers, advocates, lawyers, and clinicians frequently work with HIV-positive individuals and in the field of HIV prevention and treatment; it is vital that they understand both the medical and complex social realities faced by their clients.
Born out of a grassroots movement to combat the HIV/AIDS crisis in A&PI communities in the late 1980s, the A&PI Wellness Center works to address the health needs of marginalized and vulnerable groups, regardless of race, ethnicity, gender identity, sexual orientation, or immigration status. In collaboration with Project Inform, the A&PI Wellness Center developed the California Statewide Training and Education Program (CSTEP), a curriculum that sets the standard in HIV treatment and technically and culturally competent training for clinical and non-clinical providers working in the HIV field.
An eLearning Solution
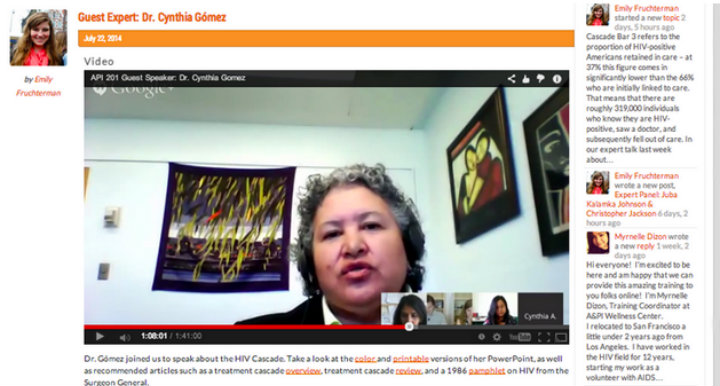
Participants will advance to APIWC 201 upon completion of the first course (APIWC 101). Hosted on TechChange’s facilitated course platform, this online course will provide more in-depth information about barriers to care and supporting clients in a dynamic era of HIV treatment. The month-long 201 course integrates elements of the self-paced course into the facilitated learning environment – participants are able to review the 101 content as well as slides specifically produced for the 201 course, share their knowledge with other providers in the forums, and interact with experts during live events. The ability to work with experts is what really sets this training apart – participants hear from former presidential advisors on HIV policy, specialists in linking HIV-positive people to care, HIV trainers, and those with decades of experience researching the virus and advocating for those affected.
Participants are able to engage with experts such as Dr. Cynthia Gómez (pictured above) during live events. These events are recorded and made available for later review.
The content of both courses is available 24/7 so that providers are able to take part whenever their schedules allow, while the forums and weekly live sessions add a social dimension uncommon in online learning. As all participants have some experience with HIV prevention or treatment, this course provides a unique opportunity for collaborative learning; providers can learn from the experiences of one another, share resources, and strengthen their networks of HIV prevention and treatment specialists.
In the first month alone, the training attracted over 70 participants from a variety of organizations. Additionally, the combined course has little in the way of overhead costs and can easily be repeated or scaled for different audiences, making it a viable strategy for training providers across California, with the goal of improving health outcomes and supporting HIV-positive individuals as they move toward viral suppression.
To register for these free online courses on HIV prevention training, please click here.
Charlie Weems and Emily Fruchterman of TechChange record a live session at the TechChange recording studio in Washington, DC.
Emily Fruchterman, Catherine Shen, Charlie Weems, and the A&PI Wellness Center contributed to this blog post.
If your organization is interested in developing online training with TechChange, please contact info@techchange.org.