Before the recent Ebola outbreak, the terms “contact tracing” and “Ebola” were spoken by only a small community of public health specialists consisting of infectious disease physicians and epidemiologists. As total cases of Ebola Virus Disease reported by the Centers for Disease Control and Prevention (CDC) exceed 10,000 across Guinea, Liberia, and Sierra Leone – almost 5000 of those fatal – these terms are increasingly entering general conversation.
What is Ebola contact tracing?
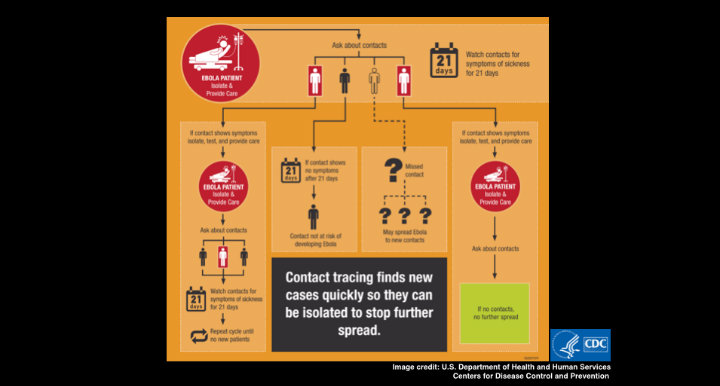
Rapid contact tracing is essential to the identification and isolation of symptomatic cases of Ebola disease, interrupting secondary transmission, and slowing exponential spread of the virus. It involves identification, documentation, and monitoring of all individuals who have come in contact with a single symptomatic case. In many cases, this is an analogue process of recording data on paper case notification, contact follow-up and field report forms, transporting those to a data entry center, and entering them into an electronic database. In other cases, mobile device can be used in the field for direct data entry into an electronic database.
Contacts have been exposed and are at risk for developing Ebola disease, but have yet to show symptoms. This is where understanding a few basics about Ebola virus and disease is helpful.
-
Transmission: direct contact with the body fluids of someone, ill or deceased, with symptoms of Ebola disease; or contact with objects contaminated by their body fluids
-
Symptoms: fever, headache, diarrhea, vomiting, stomach pain, unexplained bleeding or bruising, and muscle pain developing up to 21 days after exposure to the virus
If a contact develops symptoms within the 21 days of monitoring, they are immediately isolated and contact tracing begins for this new symptomatic case.
Ebola and Contact Tracing
Contact tracing can get complicated, so much so that the CDC has a dedicated program, the Epidemic Intelligence Service, to build US health professional capacity and expertise to do so. A single Ebola case can result in the need to trace numerous contacts. In the early outbreak stages, rapid response is most critical as contact tracing efforts are somewhat manageable. If not contained, exponential transmission can make contact tracing efforts unwieldy, as is the case in the current West Africa Ebola outbreak.
Why is it so difficult to integrate mobile phones for contact tracing?
Several challenges in contact tracing could potentially be addressed with mobile solutions. Given wide geographic spread, remote locations and limited resources, real-time data collection and monitoring with mobile phones could facilitate rapid alert of new cases and contact follow-up. These tools could reduce time lag between data collected in the field and response, and serve as a more relevant basis for assessment and prioritization of control interventions. Given that solutions are developed with the Principles for Digital Development in mind, particularly open standards, open data, and open source software, the use of mobiles could address asynchronous data collection and reporting while lowering barriers to stakeholder collaboration.
Irrespective of the integration of mobile devices, contact tracing in Guinea, Sierra Leone and Liberia presents challenges unique from those in which the methods were developed. How do you identify and quarantine an affected patient effectively in a culture where many objects – from mattresses, toilets and food, to the burden of caring for the ill– are shared? How can reliable data be collected if interviewees intentionally misdirect or misinform surveillance officers in fear of response efforts? Social behavioral change communication could address these challenges, with mobiles playing a role.
Several groups are currently working to address data related issues in the West Africa Ebola outbreak. Notably, the World Health Organization’s Harmonized Ebola Response built on the Ona platform, the Ebola Open Data Jam, and mHero, a collaborative effort partnering IntraHealth International’s iHRIS software and UNICEF’s mobile messaging platform RapidPro. Three initiatives running in parallel leave one questioning if any single effort is actually impacting harmonization?
The challenges hindering rapid integration of mobile solutions are not necessarily unique from larger challenges in implementing mobile solutions, nor aid for that matter. Do you understand the user and ecosystem, did you design for sustainability and scale, and did you leverage opportunities for collaboration? There are suggestions that the WHO and mechanisms for responding to global health challenges are outdated, positioning the West Africa Ebola outbreak as a defining moment in their reevaluation. Perhaps it will also bring new perspective to effective leverage of mobile solutions.
Are you a “healthie”, “techie” or someone in-between interested in the use of technology in global health? Then don’t miss your chance to join course facilitator Kendra Keith and the next cohort of TC309: Mobiles for Public Health starting November 17th, 2014!